Chapter 13 of Get Hip! deals with managing pain. I have seen questions about pain management on Twitter, so I’m sending this to reach more hip replacement patients.
–Rob
Before my surgery, I decided I would use as little anesthesia and narcotic pain medication as possible. I figured my threshold for tolerating pain was pretty high, and opioid abuse was then ravaging my home state of New Hampshire, leaving a trail of overdose deaths, neglected kids and infants born with addiction. Nationally, opioid overdose deaths had tripled in 15 years. I didn’t want to join that crowd.
The one Tramadol pill I took my first night home was the last I ever took. My pain level was low, and when I did have some, non-narcotic Tylenol and Naproxen seemed to deal with it.
The hospital had sent me home with 71 tablets of Tramadol, with instructions to take one every four hours, as needed. So I had 70 tablets left over, which seemed like a deplorable waste. More important, it seemed like an invitation to abuse narcotics.
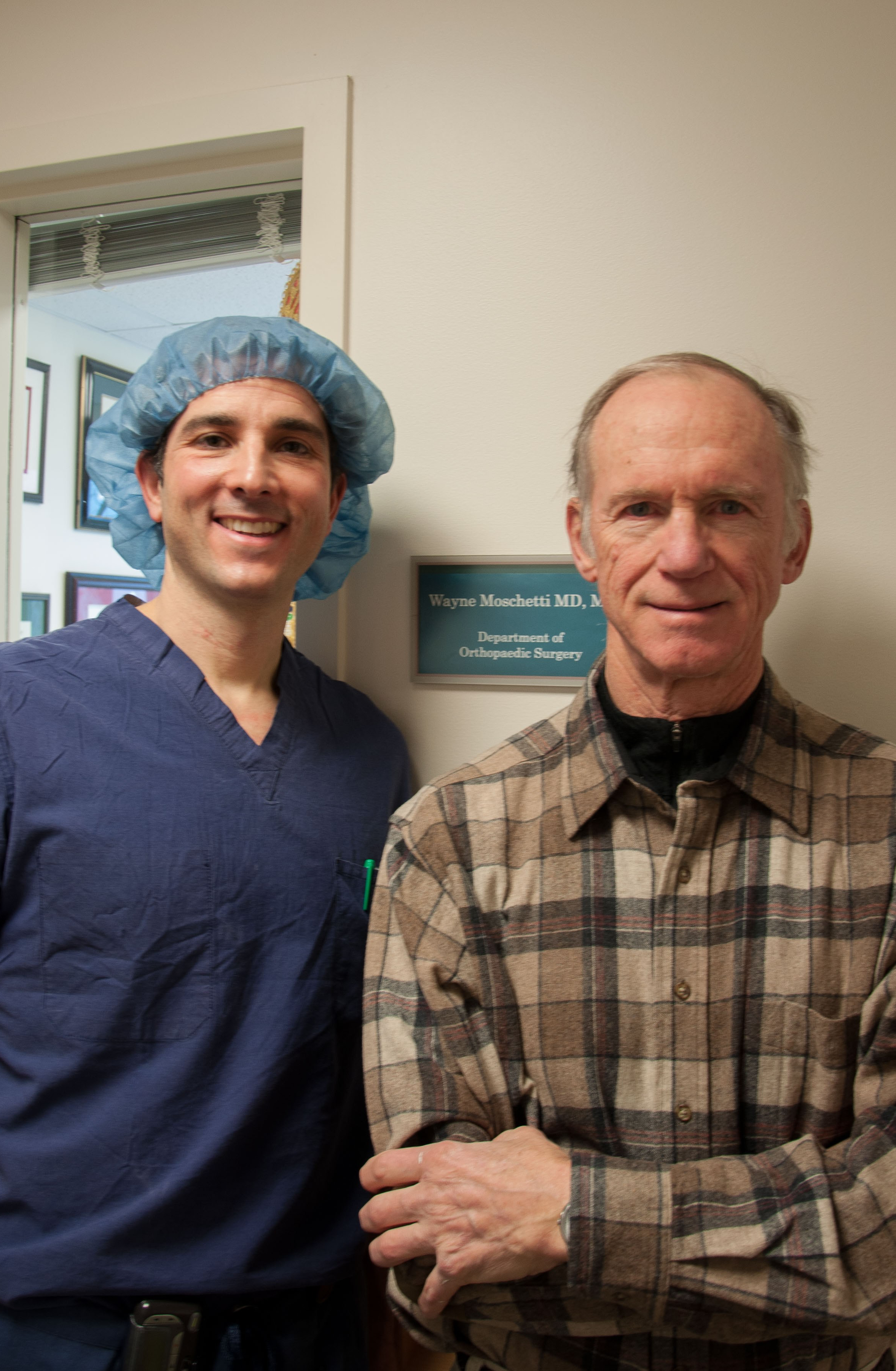
Moschetti told me that the hospital had given me the amount that an average hip or knee replacement patient had required in the past. He maintained that I was very unusual in taking only a single pain pill. Tramadol was the weakest narcotic they prescribed, he said, and I was assigned a low dose rate. That suggested that most patients used much more Tramadol or more-potent narcotics like Oxycodone or Dilaudid.
My interviews didn’t suggest I was all that unusual. Almost all the hip replacement patients I interviewed said they took their narcotics for only a day or two.
To be sure, pain is tough to pin down. Lacking any objective pain yardstick, Moschetti noted, doctors rely on patients’ evaluations of how much pain they feel and how much narcotic they need to alleviate it. And since drugs work differently on different people, predicting a drug’s effectiveness and needed dose is doubly hard.
Opioid drug makers have spent freely to convince doctors that their pills are relatively safe and non-addictive. Some currently face lawsuits claiming they made false and misleading statements.
Frankly, physician convenience and past attitudes may encourage over-prescription. It’s easier for doctors to prescribe more pills at one time than to deal with repeated patient requests for more. Doctors also want to get good patient-satisfaction scores, which may affect their compensation. “Overprescribing drugs improves patient satisfaction, but does not improve health,” said Brian Sites, my anesthesiologist.
Ten years ago, physicians were criticized for failing to help people relieve pain, which some considered the “5th vital sign.” Some said patients should have no pain, even with surgery. This attitude may have contributed to the current opioid epidemic, but it is changing.
Other conditions may have a bearing on sensitivity to pain or vulnerability to addiction. One study co-authored by Dr. Sites disclosed that individuals with mental disorders used opioids at more than triple the rate of other Americans. The study concluded, “Improving pain management among this population is critical to reduce national dependency on opioids.” 27
Avoiding Dependence
One study found narcotic dependence in 15 to 26 percent of patients who got opioids. Spurred by such findings, the American medical world is looking more skeptically at whether patients need narcotics.28 A recent study of emergency departments found no significant difference between the short-term pain relief provided by opioids and non-opioid analgesics like ibuprofen (Advil) and acetaminophen (Tylenol).29 With addiction, as with disease, prevention is easier than treatment. A Journal of the American Medical Association editorial said that substituting non-opioid treatments for pain may prove to be an important step toward reducing opioid addiction.30
At DHMC, pain management experts from the anesthesiology department working with the orthopedic surgery department have created a comprehensive approach that offers multiple options for pain management in addition to opioids.
Guideline Fourteen: Try to Get by With Minimal Narcotics
I did. So did most of the patients I interviewed. Icing the hip and taking non-steroidal anti-inflammatories can often relieve pain and don’t constipate you, as do narcotics. Medicine is moving fast toward using opioids less frequently than in the past, which may reduce addiction.
 Some hip replacement patients worry that they’ll be left with a big, ugly scar. I bring good news. I wasn’t.
Some hip replacement patients worry that they’ll be left with a big, ugly scar. I bring good news. I wasn’t.